- April 20 2022
- Fast Focus Policy Brief No. 58-2021

Pre-release Medicaid enrollment assistance helps formerly incarcerated individuals navigate the reentry process. Removing barriers to outpatient healthcare needs and improving access to basic medical services are of particular importance for those with histories of substance use. It may also help reduce high rates of post-release illness and overdose death in the initial weeks following release from prison.[1]
While about 58% of incarcerated adults in state prisons meet the clinical criteria for drug dependence or abuse,[2] less than 30% of those individuals receive any drug-use treatment while incarcerated (with less than 0.5% receiving pharmaceutical treatment). Amid a nationwide opioid crisis, increasing access to health care for those navigating reentry is prioritized in both the Medicaid reentry provision of the 2018 Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act[3] and the proposed Medicaid Reentry Act of 2021.[4]
A research team led by Marguerite Burns, an Institute for Research on Poverty (IRP) Affiliate and UW–Madison Associate Professor of Population Health Sciences, looked to build on previous work which found evidence that pre-release Medicaid enrollment assistance effectively increased Medicaid enrollment (see Figure 1).[5] Their follow-up study, discussed below, asks whether prison-based Medicaid enrollment assistance is associated with increased use of health care within 30 days of prison release among adults with a history of substance use.[6]
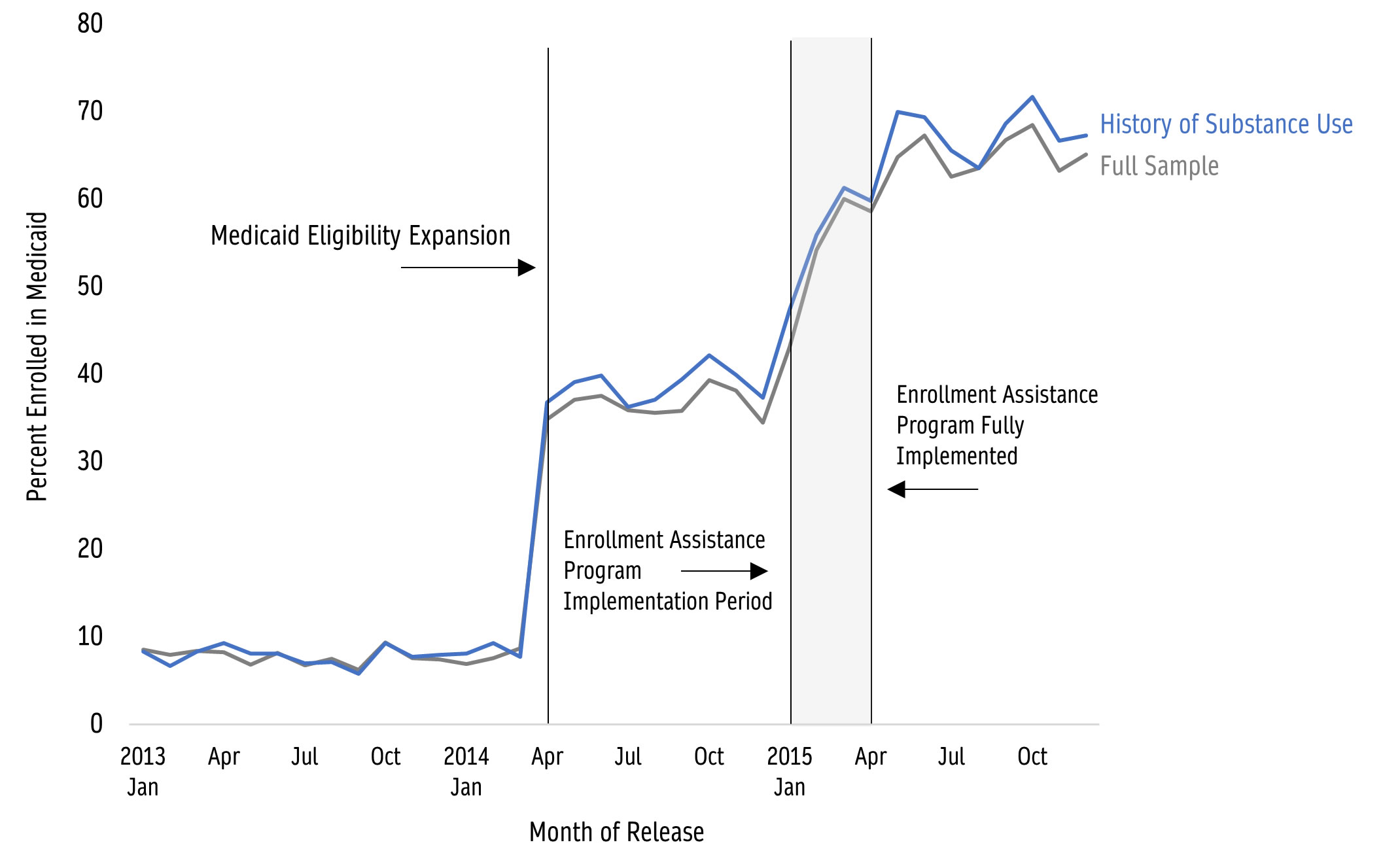
Source: Burns, M.E., Cook, S., Brown, L., Tyska, S., Westergaard, R. (2021, Aug.). Increasing Medicaid Enrollment among Formerly Incarcerated Adults. Health Services Research, 56(4): 643–654. DOI: 10.1111/1475-6773.13634
Background and Data
In Wisconsin, Medicaid coverage is available to adults with incomes below 100% of the poverty line, which includes most adults leaving prison. In January 2015, the Wisconsin Department of Corrections (DOC) began a program of pre-release Medicaid enrollment assistance for adults in state correctional facilities. The initial process involves facility-based discharge planners guiding prisoners on how to apply for Medicaid; individuals can then contact external case workers to confirm eligibility and apply for Medicaid coverage. In some facilities, paralegal benefits specialists are also available to assist with the enrollment process.
Data for this project were drawn from several Wisconsin state agency databases, including IRP’s Wisconsin Administrative Data Core. History of substance use was also determined through sources such as self-reported opioid use and DOC assessment tools. The total number of observations in this study was 18,265 releases among 16,307 incarcerated individuals (89.4% male; 60.1% white). To assess the effectiveness of the program, researchers developed a retrospective cohort study and compared pre- and post-implementation outcomes. The research team evaluated four binary (i.e., yes/no) outcomes related to Medicaid-supported outpatient care within 30 days of prison release: Any outpatient visit; a visit associated with any substance-use disorder (SUD); a visit associated with any opioid use disorder; and receipt of medication for opioid use disorder.
Key Findings
Three key findings emerged. First, the presence of a pre-release Medicaid enrollment assistance program was associated with a large overall increase in the likelihood of individuals taking part in outpatient visits within 30 days of release. Outpatient visits of any kind among adults participating in the pre-release enrollment assistance program rose from 16.1% at baseline to 24.4% after the program was implemented.
Another key finding was that despite relative increases in SUD-related outpatient visits, overall levels of post-incarceration health care use for substance use disorders remained low. Put another way, the pre-release enrollment program appears to have helped increase access to post-incarceration healthcare within the first month after release, but overall, recently released individuals with substance use histories do not often seek medical attention for substance use treatment. Burns and her team suggest that ongoing barriers to greater healthcare access may include limited health literacy;[7] competing priorities among recently released individuals, including family and financial priorities;[8] and logistical challenges[9] that may vary widely across individuals and community contexts. Transitional care clinics are one important component for easing the burdens of reentry. These clinics help foster supportive community connections and information-sharing among professionals working to assist those navigating reentry.
A third key finding was that there is no evidence to suggest reductions in the use of hospital-based care (including Emergency Room visits) among the study population. For adults with SUD, quick connection to treatment options upon release from prison may be lifesaving by preventing unintended overdose. Burns and her colleagues suggest that individuals with high overdose risk may be less likely to seek outpatient treatment without substantial additional support or intervention (beyond simply having health insurance).
The results of this study affirm the catalytic role of pre-release Medicaid enrollment assistance for reducing barriers to healthcare access in the initial weeks following release from prison. Yet, as Helen E. Jack, MD, writes in her invited commentary,[10] this study “shows us that Medicaid enrollment assistance may be necessary, but is not sufficient, for supporting people releasing from prison to link with community-based health care services.” It is crucial, Jack says, that “research and implementation efforts consider the social and structural determinants of health that recently released patients face.” Homelessness, poverty, racism, and discrimination due to criminal history, can all be “barriers to accessing care and may contribute to poor health outcomes.”
While pre-release enrollment assistance was a useful policy change—and increasingly available nationwide—Dr. Jack suggests that such community-based interventions place “insufficient burden” on both correctional institutions and policymakers. Burns and colleagues test the effectiveness of this Wisconsin-based intervention, says Jack, but other “policy changes may be needed for new programs… to be implemented at scale.”
Policy Considerations
Until October 2020, Wisconsin terminated (rather than merely suspended) Medicaid coverage for incarcerated individuals. Medicaid suspension temporarily deactivates coverage while a person is incarcerated.[11] Compared to outright termination of coverage, suspension allows for more efficient renewal of Medicaid upon release. To avoid lapses in coverage due to uncertain release dates, delayed eligibility determinations, and other administrative considerations, incarcerated individuals and carceral systems nationwide will be better served by making suspension (rather than coverage termination) and pre-release Medicaid enrollment assistance universally available as common practice.
Implementing the Medicaid reentry provision of the 2018 SUPPORT for Patients and Communities Act is also important. The Medicaid Reentry Act (Sec. 5032) states, in part, that the Centers for Medicaid and Medicare Services “must convene a stakeholder workgroup in order to develop best practices for states to help inmates released from public institutions transition to the community with health care (such as by ensuring continuity of health insurance or Medicaid coverage).”
Collaboration is a key to success in policy and practice. As this study shows, it will take the collective will of community-based clinicians, policymakers, correctional facilities, and researchers to understand and implement effective policy such as making pre-release Medicaid enrollment assistance universally available within correctional settings nationwide.
[1] Bukten, A., Stavseth, M.R., Skurtveit, S., Tverdal, A., Strang, J., Clausen, T. (2017). High risk of overdose death following release from prison: variations in mortality during a 15-year observation period. Addiction, 112(8), 1432-1439. DOI: https://doi.org/10.1111/add.13803
[2] Bronson, J., Stroop, J., Zimmer, S., Berzofsky, M. (2017, June). Drug use, dependence, and abuse among state prisoners and jail inmates, 2007-2009. Bureau of Justice Statistics, US Department of Justice. https://bjs.ojp.gov/content/pub/pdf/dudaspji0709.pdf
[3] Substance Use-Disorder Prevention That Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act. HR 6 (2018). https://www.congress.gov/bill/115th-congress/house-bill/6
[4] Medicaid Reentry Act of 2021. HR 955, 117th Congress (2021-2022). https://www.congress.gov/bill/117th-congress/house-bill/955
[5] Burns, M.E., Cook, S., Brown, L., Tyska, S., Westergaard, R. (2021, Aug.). Increasing Medicaid Enrollment among Formerly Incarcerated Adults. Health Services Research, 56(4): 643-654. https://doi.org/10.1111/1475-6773.13634
[6] Burns, M.E., Cook, S., Brown, L.M., Dague, L., Tyska, S., Hernandez Romero, K., McNamara, C., Westergaard, R.P. (2022). Association between assistance with Medicaid enrollment and use of health care incarceration among adults with a history of substance use. JAMA Network Open, 5(1), e2142688. https://doi.org/10.1001/jamanetworkopen.2021.42688
[7] Hadden, K.B., Puglisi, L., Prince, L., et al. (2018). Health literacy among a formerly incarcerated population using data from the Transitions Clinic Network. Journal of Urban Health, 95(4), 547-555. https://doi.org/10.1007/s11524-018-0276-0
[8] Western, B., Braga, A.A., Davis, J., Sirois C. (2015). Stress and hardship after prison. American Journal of Sociology, 120(5), 1512-1547. https://doi.org/10.1086/681301
[9] Mallik-Kane, K., Paddock, E., Jannetta, J. (2018, Feb.). Health Care After Incarceration: How Do Formerly Incarcerated Men Choose Where and When to Access Physical and Behavioral Health Services? Urban Institute. https://www.urban.org/research/publication/health-care-after-incarceration
[10] Jack, H.E. (2022, Jan. 7). Medicaid enrollment assistance for people released from prison—One step on a long road. JAMA Network Open, 5(1), e2142695. https://doi.org/10.1001/jamanetworkopen.2021.42695
[11] Congressional Research Service. (2021, May 12). Medicaid and Incarcerated Individuals. In Focus. https://crsreports.congress.gov/product/pdf/IF/IF11830
Categories
Health, Health Care, Incarceration, Justice System, Mental Health & Substance Abuse, Prisoner Reentry
Tags
Medicaid, Natural Experiment, Substance Abuse (or Alcohol/Drug Abuse), Wisconsin